Entries by Scott McPherson (423)
Three more Indonesian H5N1 human positives
 It is dang difficult trying to understand what is going on in Indonesia these days. That is one reason why I am also adjusting to the H5N1 "New Normal" that I blogged about a few weeks ago. Reports of "hot high" -- machine translation for high fever -- abound in the Indonesian press.
It is dang difficult trying to understand what is going on in Indonesia these days. That is one reason why I am also adjusting to the H5N1 "New Normal" that I blogged about a few weeks ago. Reports of "hot high" -- machine translation for high fever -- abound in the Indonesian press.
Most of these accounts wind up testing negative, or so we are told. Many of us are dubious whenever we hear about negative tests. Our skepticism was reinforced via yesterday's WHO report on the Pakistani family cluster of last October and November. Curious that it took so long to confirm what we already suspected.
The latest WHO report from Indonesia speaks of three confirmed human H5N1 infections. Two are from West Java; one is from West Sumatra. All are young. Two are dead.
What is beginning to percolate up from the local press, captured and analyzed by our worldwide team of flubie lay translators and geographers (you know who you are), is that two of the latest H5N1 cases are related to family members who also complained of "flu-like" symptoms at the same timeframe to suggest human-to-human -- or H2H -- transmission. First, the WHO official update.
Avian influenza – situation in Indonesia – update 41
2 April 2008
The Ministry of Health of Indonesia has announced three new cases of human H5N1 avian influenza infection. The cases are not linked epidemiologically. The first is a 15-year-old male student from Subang District, West Java Province who developed symptoms on 19 March, was hospitalized on 22 March and died on 26 March .
The second case is an 11-year-old female student from Bekasi City, West Java Province who developed symptoms on 19 March, was hospitalized on 23 March and died on 28 March.
The third case is a 21-month-old female from Bukit Tinggi, West Sumatra Province who developed symptoms on 17 March, and was hospitalized on 22 March. She is presently recovering in hospital.
The source of infection for all three cases is still under investigation.
Of the 132 cases confirmed to date in Indonesia, 107 have been fatal.
http://www.who.int/csr/don/2008_04_02/en/index.html
Dr. Henry Niman was among the first to note that the brother of the 15-year old who died, had himself died earlier. That death was attributed to dengue fever. Strange that the first brother was not tested for H5N1, apparently. Dr. Niman's commentary is below:
H5N1 Clusters and Denials Raise Indonesian Pandemic Concerns
Recombinomics Commentary 13:50
March 31, 2008
Kandun dismissed the possibility of more bird flu cases in the same family after the boy's brother died recently. Confirmed cluster cases raise concerns over human-to-human transmission. "It is not correct that there is a cluster in Subang," Kandun said, adding that the brother has died of dengue fever.
The above denial of an H5N1 cluster in Subang is cause for concern. Both brothers were initially diagnosed as dengue fever. However, since dengue fever is transmitted by insects, they likelihood of two fatal cases in the same family with distinct disease onset dates is remote. Consequently, the second case was tested for H5N1 and was positive, strongly suggesting that the index case was also H5N1 positive and infected his brother. The denial of the cluster by the director general of communicable disease control in Indonesia raises serious transparency problems, and is similar to denials of H5N1 in the first confirmed cluster in Indonesia, almost three years ago. Those cases were initially said to have died from bacterial pneumonia, although the father was subsequently H5N1 confirmed, and the H5N1 from that patient is a target for vaccines directed to clade 2.1, the clade of H5N1 in Indonesia. (bold mine)
In addition to the death of a family member of an H5N1 confirmed case in West Java, a similar cluster has been reported in the local media in Sumatra. H5N1 has been confirmed in a young child, but the recent death of a family member has not been reported in the English language press. Similarly, the nurse who cared for one or both family member is in isolation with bird flu symptoms, raising concerns of a expanding cluster.
The two clusters above, as well as a third confirmed case, located in Bekasi, which is near the two brothers in West Java, raises pandemic concerns. Although clusters in Indonesia are not new, the government denial of the cluster in West Java and the failure of the English press to recognize the cluster in Sumatra, raises concerns that the number of cases and clusters are significantly higher than the reported confirmed or suspect cases.
More information of testing in these two clusters would be useful. Dengue fever claims raise concerns that additional H5N1 cases are being mis-reported.
http://www.recombinomics.com/News/03...er_Denial.html
So two of the most recent H5N1 cases had family members who died suddenly at about the same time. As I have maintained, in public health there are no coincidences. The possibility that family members would die of different diseases in the same timeframe is remote and not nearly as plausible as the suggestion they all died from the same thing. H5N1. And if that were true, the number of family clusters in Indonesia is accelerating even more than we have previously confirmed.
Perilous times, indeed. Perhaps the WHO should consider assigning different phases to different countries, the same way that Homeland Security assigns different warning colors to different sectors. For example, today the US is at Yellow, while air travel maintains Orange. Using that logic, who could possibly disagree that Indonesia warrants a Phase Four?
Limited H5N1 H2H "likely occurred" in Pakistan - WHO
Very quietly, the World Health Organization today confirmed what most of us had suspected all along -- that the Pakistani H5N1 human cases among family members in October and November of last year were, indeed, "likely" victims of human to human transmission.
In the April 3, 2008 Update 2, three of the four family members (all male) were confirmed to have contracted H5N1, and the fourth is unconfirmed but "probable". It is unknown if chain H2H2H transmission occurred, but judging by the onset dates, it is quite reasonable to assume this event is also likely.
Here is the WHO report, and a massive hat-tip to Crof for publishing this on his blogsite, H5N1. And here's another sigh of relief that we dodged the proverbial bullet once again.
Will our luck continue to hold out until we get real-time, global surveillance? No one on Earth can answer that one.
Avian influenza – situation in Pakistan - update 2
3 April 2008
Two additional H5N1 cases were confirmed by serological testing, thus providing final H5N1 infection test results on a previously reported family cluster in Peshawar.
These tests were conducted by the WHO H5 Reference Laboratory in Cairo, Egypt and the WHO Collaborating Centre for Reference and Research on Influenza in Atlanta, USA. The table below summarises the testing results of the confirmed/probable cases in the family cluster.
- The preliminary risk assessment found no evidence of sustained or community human to human transmission.
- All identified close contacts including the other members of the affected family and involved health care workers remain asymptomatic and have been removed from close medical observation.
These laboratory test results support the epidemiological findings from the outbreak investigation in December 2007, and the final risk assessment that suggested limited human to human transmission likely occurred among some of the family members which is consistent with some human-to-human transmission events reported previously. This outbreak did not extend into the community, and appropriate steps were taken to reduce future risks of human infections.
http://www.who.int/csr/don/2008_04_03/en/index.html
Relationship
Onset Date
Outcome
Exposure
Status
Case 1 (Index case)
29 Oct 07
Fully recovered
Direct contact sick/dead poultry
Confirmed (serology)
Case 2
12 Nov 07
Dead (19 Nov 07)
Close contact with Case 1, no known direct contact with sick/dead poultry
Probable
(No sample available)Case 3
21 Nov 07
Dead (28 Nov 07)
Close contact with Case 1 and 2, no known direct contact with sick/dead poultry
Confirmed (PCR)
Case 4
21 Nov 07
Fully recovered
Close contact with Case 1 and 2, no known direct contact with sick/dead poultry
Confirmed (serology)
Sorry the table did not transfer all the columns. Please click on the link to view the entire table directly from the WHO.
SCott
One possible explanation for bizarre celebrity behavior
I just had to post this. Story speaks for itself.Botox May Move From Face to Brain, Study in Rats Says (Update1)
By Elizabeth Lopatto
April 1 (Bloomberg) -- Botulinum neurotoxin type A, sold as Allergan Inc.'s Botox remedy for wrinkles, can move from its injection site to the brain, a study shows.
Scientists injected rats' whisker muscles with botulism toxin. Tests of the rodents' brain tissue found that botulism had been transported to the brain stems, the researchers said in the Journal of Neuroscience published April 2.
Botox is Allergan's biggest product, with $1.21 billion in sales last year. The drug, approved in 1989, became fashionable among aging celebrities seeking to smooth facial wrinkles and is used to treat some neurological disorders. The U.S. Food and Drug Administration is investigating whether patients contracted botulism, a muscle-weakening illness, from Botox and Myobloc, a product from Solstice Neurosciences Inc.
``The idea that there could be some transmission of this to the central nervous system needs to be followed up,'' said Mathew Avram, the director of Massachusetts General Hospital's Dermatology, Laser and Cosmetic Center, in Boston, in a telephone interview today. ``But this treatment has been used on millions of people for years, and we're not seeing major central nervous system uses with it.''
Botulism neurotoxin can disrupt nerve cells' ability to communicate and may change spinal cord circuitry, the authors wrote in the study.
Rodents, Not Humans
Mouse and rat physiology is different from that of humans, so the results may not predict what happens in people, Avram said. He wasn't involved in the study.
The study isn't conclusive, and because it contradicts previous findings, more work is necessary, according to an Allergan spokeswoman. The company is based in Irvine, California.
``The authors used a laboratory preparation of botulinum toxin and did not use Botox, and data suggest that different preparations of botulinum toxin react differently in both the laboratory and in clinical practice,'' said the spokeswoman, Caroline Van Hove, in an e-mailed statement.
Myobloc is botulinum neurotoxin type B, a different type of botulinum than studied, said Edgar Salazar-Grueso, chief medical officer of Solstice Neurosciences, in a telephone interview today.
``We are aware from monkey studies already published that toxin A migrates more than B,'' Salazar said. ``Monkeys are more like humans than rodents, so these findings we're observing are consistent.''
FDA Evaluation
Scientists injected botulism toxin into one side of the hippocampus in each rodent brain, and into their superior colliculus, a visual center. From one side of the hippocampus, the toxin migrated to the opposite. From the visual center, the drug went to the animals' eyes.
The effects of the injection into the hippocampus were still present six months later, the scientists wrote.
The FDA is evaluating reports of breathing difficulties and death after use of Botox and Myobloc, according to a posting in February on the agency's Web site. Many of the most serious cases involved children who received the injections to treat arm and leg spasms associated with cerebral palsy, a use not approved by the FDA.
Prescribing literature for Botox and Myobloc now carries warnings about the risk of breathing and swallowing difficulties in patients with neuromuscular disorders. The FDA said the new data suggest that life-threatening side effects may occur in patients with other conditions, including children with cerebral palsy.
Large Doses
Higher doses of Botox are injected to treat limb spasms in children with cerebral palsy in about 60 countries. Some U.S. doctors use it for this purpose, though Allergan doesn't market it in the U.S. for the unapproved use. A typical cosmetic dose is about 10 times less than a dose for cerebral palsy, Avram said.
``The FDA was investigating Botox in situations where large amounts were used,'' Avram said. ``Those tend to be very young children with massive doses. I don't know that this study relates to that.''
Botulism, which can also be spread through contaminated food or wounds, is caused by a bacterium called clostridium botulinum, according to the U.S. Centers for Disease Control and Prevention, in Atlanta. About 110 cases are reported in the U.S. each year.
http://www.bloomberg.com/apps/news?pid=20601124&sid=a4B_t.tm4Kpc&refer=home
It's not always influenza that kills, part 4
 A bacteria almost as lethal and more difficult to kill than MRSA hitches a ride home on military personnel.
A bacteria almost as lethal and more difficult to kill than MRSA hitches a ride home on military personnel.
The London (UK) Daily Mail is reporting in today's editions about acinetobacter, possibly the nastiest bacteria on the planet. I'll let you read the article first, then scroll down.
Pandemic warning over the hospital superbug that resists safe antibiotics
Last updated at 00:00am on 1st April 2008
Doctors fear a pandemic of a lethal hospital superbug that is even more drug resistant than MRSA.
Staff battling outbreaks of acinetobacter are having to resort to antibiotics sidelined 20 years ago because of fears about their safety.
Even these do not always work, raising fears that the bacterium commonly found in soil and water could become uncontrollable.
Acinetobacter expert Professor Matthew Falagas said: "In some cases we have simply run out of treatments and we could be facing a pandemic with important public health implications."
More than 1,000 Britons catch acinetobacter every year. It is normally harmless, but can cause blood poisoning and life-threatening pneumonia in the vulnerable.
There are no official figures on fatalities but the superbug was linked to 39 deaths at St Mary's Hospital in Paddington, West London, three years ago. (bold mine)
It is thought many infections stem from soldiers returning from the Iraqi and Afghan deserts.
In 2003, 93 patients, including 91 civilians, were infected at Birmingham's Selly Oak Hospital, where servicemen were being treated on the same wards as other patients.
Thirty-five of those infected with acinetobacter died but the hospital was unable to establish if the bug was the main cause of death. (bold all mine)
Speaking at a Society for General Microbiology conference in Edinburgh, Professor Falagas warned that doctors were running out of options to treat acinetobacter. He said: "Doctors in many countries have gone back to using old antibiotics that were abandoned 20 years ago because their toxic side-effects were so frequent and so bad.
"But superbugs like acinetobacter have challenged doctors all over the world by now becoming resistant to these older and considered more dangerous medicines.
"Even colistin, an antibiotic discovered 60 years ago, has recently been used as a salvage remedy to treat patients with acinetobacter infections.
"And it was successful for a while but now it occasionally fails due to recent extensive use that has caused the bacteria to become resistant."
In contrast, MRSA, the bug more commonly associated with antibiotic resistance, is easier to treat.
Acinetobacter can survive on floors and furniture for almost three weeks. It tends to attack the seriously ill, such as cancer sufferers, car crash victims and burns patients.
The Health Protection Agency advises hospitals to isolate infected patients.
After the patient leaves, the ward should be thoroughly cleaned, with bedding disinfected or even thrown away to prevent further spread.
• Bacteria-killing viruses in medical products are being tested as a weapon against MRSA.
The "assassin" viruses, which are harmless to humans, breed inside MRSA bugs and kill them as they burst out.
Tests have been so successful that virus-packed stitches, dressings and detergents could be on the market in as little as a year.
Acinetobacter has been fingered as hitching a ride to the UK and the US via wounded soldiers and servicemen and women returning home from tours of duty in Iraq and Afghanistan. According to the website dedicated to awareness about the bug, http://www.acinetobacter.org/, this is becoming more and more common. This disease has also gotten the attention of such respected organizations as The American Legion. The following is from the March, 2008 issue of American Legion magazine:
Medical experts wary of dangerous germ now striking war‑wounded troops.
THE IRAQIBACTER
BY MARGARET DAVIDSON
Staff Sgt. Nathan Reed was escorting a CBS news team through Baghdad for a Memorial Day visit in 2006 when the car bomb went off. Reed survived, but his right leg was severely injured. He was rushed to military hospitals in Iraq and Germany, then to Brooke Army Medical Center in San Antonio.
The injured leg developed an infection from a bacterium called acinetobacter baumannii. Reed had to decide whether or not to have his leg amputated. He consulted his doctors. He weighed his options. Finally, after getting all the information he could, he went ahead with the surgery. "The Iraqibacter pretty much sealed the fate for my amputation," he says.
The bacterium nicknamed the Iraqibacter is an increasingly multi-drug-resistant supergerm that is plaguing wounded soldiers who served in Iraq. The Infectious Diseases Society of America (IDSA) has put it on a short list of six dangerous, top-priority, drug-resistant microbes. Doctors are running out of ammunition to fight it.
The Iraqibacter joins on that list a better-known and more common supergerm, methicillin-resistant staphylococcus aureus (MRSA). Though less virulent than MRSA, acinetobacter baumannii is more drug-resistant. Not only does it possess a number of resistant genes itself, it also accepts resistant genes from other bacteria.
"I think it's unique," says Col. Glenn Wortmann, acting chief of infectious diseases at Walter Reed Army Medical Center, about the Iraqibacter's resistance, "and I think that's what has the IDSA so concerned."
Many infected soldiers respond to only a couple of different drugs. And Wortmann says he has encountered one or two isolated lab samples of the bacteria that were resistant to all antibiotics. "The issues with acinetobacter resistance are likely to continue to grow," predicts epidemiologist Arjun Srinivasan of the Centers for Disease Control and Prevention.Acinetobacter (pronounced a-sin-EE-toe-back-ter) has quietly become a new cost of war in terms of the added time it takes infected soldiers to recover, the deaths of a few infected individuals, and the resources involved in treatment and prevention.
How widespread is the problem? Military and CDC representatives say they don't know because acinetobacter cases are not required to be reported. (bold mine)
Online bloggers accuse military officials of not being forthcoming about the extent of the problem. "They've done everything they can to play down the numbers," charges one of those bloggers, veteran activist Kirt Love, who is director of the Desert Storm Battle Registry.
One expert on the Iraqibacter, Maj. Clark K. Murray of Brooke Army Medical Center's Infectious Disease Service, disagrees. "We have published a large body of scientific work on the bacteria and have discussed with numerous media sources the impact of acinetobacter," he says.
Numbers are hard to pin down, but studies of U.S. military hospitals document a dramatic increase since the beginning of the war. For instance, at Brooke, 30 of the 151 injured soldiers from the Iraq and Afghanistan wars admitted to the hospital from March 1, 2003, to May 31, 2004, were infected with acinetobacter, up from only two infected soldiers seen there in the previous 14 months.
As case numbers surge, doctors face a declining number of treatment options because, Murray says, "the resistance of acinetobacter to antibiotics has increased over the war." Healthy individuals are at little risk, and young, physically fit soldiers are usually able to overcome the infection with the help of antimicrobial drugs that still work. But more vulnerable civilian patients in the same medical facilities have occasionally not been so lucky. Experts are divided as to what extent the Iraqibacter causes deaths. They say it is difficult to determine whether patients die as a result of the bacterial infection or from their underlying injuries or illnesses.
The bacteria can create a variety of problems, including pneumonia or meningitis and infections of the wounds, bloodstream, urinary tract or bones.
The source of the bacteria is a mystery. Types of acinetobacter bacteria occur naturally in soil and water worldwide.
However, much of the transmission of the bacteria to wounded soldiers seems to have occurred in military medical facilities. Military procedures now call for isolating and screening all incoming wounded from Iraq for acinetobacter. Strict rules of hygiene are observed to fight the bacteria, which can survive on surfaces for weeks. VA hospitals have similar requirements.
"This has the potential to become a serious problem in military and veterans hospitals, where soldiers returning from active duty worldwide are treated in the same environment as other patients," warns an article in the Journal of Clinical Microbiology.
However, the increasing drug resistance of a variety of bacteria is "not just a military problem," Wortmann says. "This is a problem that is
multinational."Margaret Davidson is a writer who specializes in medical issues.
http://www.legion.org/national/divisions/magazine/release?id=46
While the British have some pretty good stats regarding infection, I am at a loss to find comparable stats for the US. Perhaps someone can find numbers. Outside of the military, which always keeps meticulous details of diseases affecting its people, I cannot find any statistics for morbidity nor mortality. However, I do not think we are too far removed from the British example.
So why don't we demand better fact-gathering? As with adenovirus and MRSA, acinetobacter apparently does not warrant such time and effort. This should not be so: With so many people coming home from Iraq and Afghanistan with injuries and wounds, returning home to almost every town and city in America, and requiring continuing and ongoing medical care, why don't we keep better civilian statistics? We already know that hospitals are excellent breeding grounds for all sorts of communicable diseases. Soldiers, sailors, air force and Marine personnel are frequenting these medical facilities. And this is not a simple infection: This is major-league, killer bacteria we are talking about. This is stuff that makes MRSA look like a paper cut. Although MRSA is a badder bacteria, at least there are drugs that can wipe MRSA out. Today, at least. Acinetobacter, on the other hand, is less lethal, but is almost indestructible, so its bottom line is much worse than MRSA's. Plus, as you just read, it has a nasty habit of assimilating the nastiest habits of other bacterias.
There is an old saying I picked up at IBM: You Don't Know What You Don't Know. And we Don't Know the extent of penetration by acinetobacter into our communities, just like we Don't Know the penetration rate of adenovirus and MRSA. Just a few days ago, an outbreak of a "staph" infection occurred at a private clinic here in Tallahassee. The local health department was very quick to tell the community what it wasn't: It wasn't MRSA.
Great. So what is it? My guess is that in every community in America, similar stories and quick protestations of what it isn't are taking place. So let's find out what it is. And let's do a better job of tracking this most unwelcome present unwittingly brought home by our most welcome citizens, our returning military.
Follow the Money (and the PPEs)
US steps up efforts to fight bird flu in SE Asia
The US government has recently stepped up efforts to combat a potential influenza pandemic whose origins are almost certainly going to be somewhere in Southeast Asia.
I have always said that in the fight to contain pandemic influenza, as in law enforcement, Follow the Money. And Follow the Tamiflu. Nowhere was that more evident than in the efforts of the US, Indonesian authorities and the WHO to contain what appeared to be an outbreak of human H5N1 in Cikelet, West Java, in August, 2006. More than 2,000 villagers from all adjacent hamlets were placed on Tamiflu as a precaution. The story can be recalled by clicking on the reference at Crof's H5N1 blog entry from that time, "Drenching Cickelet in Tamiflu", here.
The US had shipped a substantial quantity of Tamiflu into the theater of operations some weeks before, which made quick distribution of Tamiflu possible.
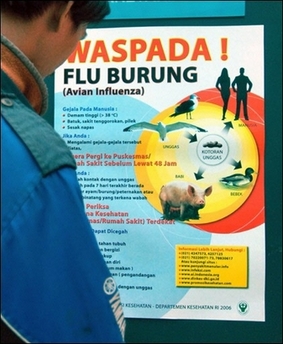
As we all know, Tangerang, Indonesia is just about the hottest spot in the world for catching bird flu, if you are a human being. And there is precious little people know there about bird flu, despite the well-intended efforts of the Indonesian government to make them more aware. I refer again to a blogger and respondent to one of my recent Computerworld.com blogs, a man known only as H&T:
I live in bird flu central (Indonesia). My wife is Indonesian and hails from a rural background in east Java. Traveling in that part of the world I am struck by two things related to bird flu:
1) Everyone keeps chickens and ducks in their yard;
2) Almost no one has any inkling about bird flu or what precautions to take (almost everyone is a subsistence farmer with little access to or interest about information on global events and concerns). (bold mine)Bird flu is almost certainly coming soon to a theatre near you. It will almost certainly "made in Indonesia" stamped on the side.
Apparently that message is not lost on the US, which is acting to try and stamp out H5N1 in Tangerang before it is too late. The United States has announced it is spending some $15 billion Rupiah, or roughly $1.7 million dollars US, to increase awareness of H5N1 in Tangerang Province alone. The following news article is from Indonesia's Antara news service:
US envoy to give Rp15 bln to Tangerang to fight bird flu
Tangerang (ANTARA News) - US Ambassador to Indonesia Cameron R Hume is expected to hand Rp15 billion in humanitarian aid to the Tangerang administration to fight bird flu in the region, a local health official said on Tuesday.
"The grant will be presented by Ambassador Cameron Hume during his visit to Tangerang on Wednesday," a spokesman of the local health office, Aceh Kurniawan, said.
He said the funds would be used to control bird flu in the city and district of Tangerang by implementing a familiarization program.
The bird flu familiarization program would involve the local people and students in an effort to make them aware of the deadly disease.
Meanwhile, the chief of the Tangerang Health Office, Hani Heryanto, said the district administration already had a bird flu control program which could be implemented as soon as the US financial aid had been received.
Meanwhile, the chief of the National Committee on Bird Flu Control, Bayu Krisnamurthi said in Jakarta recently that Indonesia had suffered financial losses of Rp4.1 trillion due to bird flu (avian influenza/AI) outbreaks during 2004-2007.
Bay said in a statement that the losses were estimated based on the impact of bird flu outbreaks during 2004-2007 using the Computable General Equilibrium (CGE) model.
The impact calculated in the estimation was financial losses due to chicken culls, reduced demand for poultry products, lower chicken and egg consumption, costs incurred by farmers as well as the government for bird flu control, and the decline in the number of tourist visits.
According to Bayu, programs to control bird flu in Indonesia had shown progress, both in communication and surveillance, managing the spread of the virus in poultry and humans, as well as efforts to anticipate a possible pandemic.
The authorities would improve the control program from time to time, he said.
AI infection of poultry which was first reported in 2003 has spread fast and now poultry in 31 out of the country`s 33 provinces have been affected.
The disease has become endemic in Java, Sumatra, Bali and South Sulawesi. (*)http://www.antara.co.id/en/arc/2008/4/1/us-envoy-to-give-rp15-bln-to-tangerang-to-fight-bird-flu/
Indonesia has lost a half-billion US dollars in the past four years, all because of bird flu. And this half-billion dollars is almost wholly contained within rural, family farms. Not to mention the loss of a major protein source. When we talk about the threat of bird flu, we sometimes lose sight of the enormous financial toll this virus takes on the living. This virus has become endemic to the nation's largest and most fertile areas. Culling exacts a massive financial toll on the standard of living for those impacted by the disease's presence. It is an extremely destabilizing and draining event for the nation, which has other things to worry about: Volcanoes, earthquakes and tsunamis, Dengue fever, chikungunya virus, malaria, al Qaeda, and a paranoid health minister.
The US is not limiting its most recent anti-bird flu efforts to Indonesia. It is also building a significant depot of supplies in Thailand, to be used throughout the Southeast Asia region. From news service AFP:
The full diplomatic resources of the United States are at work in Southeast Asia. Ambassadors are involved, engaged and delivering checks and unpacking boxes of supplies. Let's hope it all helps, and it's not too late.US officials launch bird flu stockpile in Thailand
Tue Mar 25, 12:16 PM ET
US officials on Tuesday officially opened a stockpile of equipment in Thailand designed to help Asian nations react rapidly to battle outbreaks of potentially deadly bird flu.
The US ambassador to Thailand Eric John presided over the Bangkok launch ceremony for the Regional Distribution Centre (RDC), which is located in Thailand's eastern province of Chachoengsao.
"The RDC will help ensure that countries in Asia will be able to take fast action to counter avian influenza without endangering the lives of rapid-response teams," John said.
"This centre will help ensure that avian influenza outbreaks can be contained safely and efficiently," he added.
The warehouse, funded by the US government's aid arm USAID, will initially stockpile 45,000 protective suits, 400 decontamination kits, 10 laboratory specimen kits and other equipment worth a total of 548,300 dollars.
John MacArthur, infectious diseases advisor with USAID, warned that bird flu remained a serious threat in the region around the Mekong river, and said the kits could be shipped to outbreaks within 24 hours.
Authorities in Laos earlier this month reported a fresh bird flu outbreak near its northwest border with Myanmar and China, while Vietnam has so far reported five bird flu deaths this year.
The World Health Organisation has confirmed that 236 people have died worldwide from bird flu since 2003.
The H5N1 avian influenza virus mainly kills animals but scientists fear it could mutate to easily jump from human to human, sparking a global pandemic.
http://news.yahoo.com/s/afp/20080325/hl_afp/healthfluthailandus_080325161612

