Entries in Politics and government (199)
Dengue fever alert posted for South Florida
Things are moving very quickly on the dengue fever front in South Florida. Just this morning, the Ft. Lauderdale Sun-Sentinel reported that the Centers for Disease Control and Prevention (CDC) have issued an unprecedented dengue fever warning for South Florida. Here's the article:
Advisories were in effect in Broward and Palm Beach counties Thursday after health department officials announced that a Miami Beach man had come down with a suspected case of locally-acquired dengue fever.
The announcement from the Miami-Dade Health Department follows word earlier this week of what was described as a small outbreak of the exotic, mosquito-borne disease in Key West.
That prompted a warning from the federal Centers for Disease Control and Prevention that the disease, which can be serious and even fatal on rare occasions, could spread.
Candy Sims, a spokeswoman for the Broward County Health Department, said no suspected cases have been reported locally. "But we are on high alert and monitoring the situation," she said.
Earlier this week, Harold Margolis, chief of CDC's dengue branch, issued a report in which he said, "We're concerned that if dengue gains a foothold in Key West, it will travel to other southern cities where the mosquito that transmits dengue is present, like Miami.''
Health officials urged people to keep covered up and use insect repellent as precautions.
A viral disease common to the southeastern United States and the tropics, dengue fever is not spread from person to person and is seldom fatal except to the very young and elderly with other health conditions, according to health department experts.
But this outbreak is serious enough that a specialist from the CDC recently gave classes in South Florida teaching doctors and hospital officials how to recognize the disease.
Symptoms include a high fever, severe headache, a rash, and pain in bones and joints, according to the CDC. More than 100 million cases of dengue occur every year worldwide.
The Miami Beach man who is suspected of contracting the disease has fully recovered, said Miami-Dade Health Department Director Lillian Rivera. "He is doing well," she said.
A blood sample from the Miami Beach man is being tested by the state. If dengue is confirmed, it would be the first locally contracted case of the disease in Miami-Dade Countyin at least 45 years, said Rivera.
"This is not a cause for alarm; it is a cause for creating awareness that we live with mosquitoes and we need to protect ourselves," she said.
In Palm Beach County, Health Department Director Alina Alonso sent a memo to county physicians and infection control specialists on June 30, urging "enhanced surveillance" for dengue after the Key West cases had been identified.
"It is of utmost importance that suspected cases of dengue are accurately and promptly diagnosed," she wrote in the memo. "Recent travel history to the Caribbean, Central and South American countries, or Key West in a patient with the above symptoms may suggest a consideration of dengue in the differential diagnosis."
In Key West, doctors have recorded 14 cases of dengue since April, following an outbreak of 27 cases last fall. Those cases were the first recorded in the continental United States since 1945.
More recently, epidemic dengue has become more common in the tropics and subtropics, including Puerto Rico.
But the Key West cases, said the CDC's Margolis, "represent the re-emergence of dengue fever in Florida and elsewhere in the United States after 75 years."
"These people had not travelled outside of Florida," said Margolis is a statement, "so we need to determine if these cases are an isolated occurrence or if dengue has once again become endemic in the continental United States."
For the first time in five decades, dengue fever is gaining a foothold in the United States. The authorities are moving swiftly and decisively to set up the means to detect this virus and monitor its progress. This is yet another value-add from the swine flu pandemic and bird flu preparedness drills. The monitoring mechanisms to diagnose, detect and track the spread of dengue would not be so easily set into motion, had it not been for pandemic exercises and the actual swine flu pandemic itself. People should remember this, especially residents of South Florida.
Dengue fever gains beachhead in US
Several news articles are circulating today regarding the apparent re-establishment of a permanent dengue fever colony in the United States. This should not come as a surprise; I and others have been warning of the eventual and guaranteed establishment of dengue in the US for years. Nor should the location come as a surprise. Key West is a mere 90 miles from the northern coast of Cuba, and Key West (as everyone knows) sticks out into that intersection of the Gulf of Mexico and the western Caribbean Sea, via the Straits of Florida.
Two articles illustrate the re-established dengue colony in Key West.
More than 1,000 exposed to dengue in Florida: CDC
WASHINGTON (Reuters) - Five percent of the population of Key West, Florida -- more than 1,000 people -- have been infected at some point with the dengue virus, government researchers reported on Tuesday.
Most probably did not even know it, but the findings show the sometimes deadly infection is making its way north into the United States, the researchers said.
"We're concerned that if dengue gains a foothold in Key West, it will travel to other southern cities where the mosquito that transmits dengue is present, like Miami," said Harold Margolis, chief of the dengue branch at the U.S. Centers for Disease Control and Prevention.
"These cases represent the reemergence of dengue fever in Florida and elsewhere in the United States after 75 years," Margolis said in a statement.
"These people had not traveled outside of Florida, so we need to determine if these cases are an isolated occurrence or if dengue has once again become endemic in the continental United States."
Dengue is the most common virus transmitted by mosquitoes, infecting 50 million to 100 million people every year and killing 25,000 of them.
It can cause classic flu-like symptoms but can also take on a hemorrhagic form that causes internal and external bleeding and sudden death. Companies are working on a vaccine but there is not any effective drug to treat it.
Dengue was eradicated in the United States in the 1940s but a few locally acquired U.S. cases have been confirmed along the Texas-Mexico border since the 1980s. More cases have been reported recently in Mexico and the Caribbean.
After 27 cases of dengue were reported in Florida in 2009, scientists from the CDC and the Florida Department of Health took blood samples from 240 randomly chosen Key West residents.
Of these, 5 percent had active dengue infections or antibodies to the virus, showing they had been infected, the researchers told the International Conference on Emerging Infectious Diseases being held in Atlanta.
The second article is from the Sun-Sentinel, one of Florida's largest daily newspapers, headquartered on Ft. Lauderdale:
Officials warn again about dengue fever in Key West
11:02 p.m. EDT, July 13, 2010
As South Floridians motor to the Keys for summer vacation, health officials on Tuesday urged caution about the persistent presence of mosquito-borne dengue fever in Key West.
Doctors have logged 14 cases in the old town since April — two last week — after an outbreak of 27 cases last fall marked the first time since 1945 that someone got the virus in the continental United States.
No one has died, and most people don't even get sick when infected with dengue, officials said in Tuesday's report from the federal Centers for Disease Control and Prevention. But it's the first time the virus has returned for a second U.S. outbreak in the same place.
"Most experts thought it would not be back, but here it is. It has come back," said Carina Blackmore, a Florida Department of Health expert on mosquito diseases who helped write the CDC report. "We all need to be careful."
That includes the 3.3 million tourists who visit the Keys each year, 35 percent of whom are from Florida and a large share of whom come from South Florida.
Officials said tourists have little to worry about as long as they take basic precautions against bug bites: Stay indoors from dusk to dawn, wear long sleeves and pants if outside at those times, use repellent with the chemical DEET and eliminate even small pools of standing water where the bugs breed.
"I don't think people have to worry about coming to Key West. They should be aware of the outbreak, but if they stay in a hotel with air conditioning and take simple steps, their risk should be absolutely minimal," said Dr. Mark Whiteside, medical director at the Monroe County Health Department.
Aside from dengue, three horses in South Florida have died from mosquito-borne encephalitis, and a few chickens have tested positive for West Nile virus. All three diseases are carried by different mosquitoes, but officials said the need for caution is clear.
Dengue fever infects about 50 million people worldwide and kills 25,000. The symptoms can include fever, aches, pains, rash, upset stomach and vomiting. Two of those infected in the Keys were hospitalized.
Last fall, health officials took blood samples from 240 Key West residents and reported Tuesday that 5 percent had been exposed to dengue. Blackmore said the number probably has gone up.
There's little risk of the carrier mosquito — Aegus aegypti — venturing off the island. Blackmore said the species generally stays close to home. But a risk is that a visitor could get infected and then be bitten by mosquitoes at home, spreading dengue to a new locale.
"We're concerned that if dengue gains a foothold in Key West, it will travel to other southern cities where the mosquito that transmits dengue is present, like Miami" and the rest of South Florida, said Harold Margolis, dengue chief at the CDC.
For more information, see http://www.cdc.gov/dengue or call 800-232-4636.
We once had a powerful weapon to fight mosquitoes, and it was a doozy: DDT. But the advent of Silent Spring, the '60s Rachel Carson book, pretty much killed DDT like Ralph Nader killed Corvairs. Now, however, we are learning more and more about DDT. And it appears Ms. Carson took extreme liberties when it came to the effects of DDT on the environment. I am stopping short of saying Ms. Carson lied, but the effect on DDT was the same as if she had.
I head a story on the radio, and I heard a similar story from another source, and the stories prompted me to remember riding my bicycle behind the ol' fogger truck as it made its way through my old Lighthouse Point, Florida neighborhood. It was so cool to ride in the "fog" created by that machine as it lumbered through our streets! Sometimes it would back up and hit a backyard, a vacant lot, a wooded area or a construction site with more fog, upon request.
I am certain that some readers are recoiling in abject horror at that statement! But I am also confident that there are several of you out there who recall those days with fondness. Despite the recoil, let me assure you that I have no visible nor invisible scars to show for those days.
How many African children could have been saved with the re-establishment of DDT? Perhaps the million per year that die from mosquito-borne viruses? Sadly, our only answer to malaria, dengue and chickungunya (all mosquito-borne) is to buy a lot of DEET-enriched repellent and to ship mosquito nets to Africa. I shake my head at that.
Even the WHO has issued entreaties to restore the development and production of DDT. It's the only thing that reliably works on mosquitoes. And I do not believe (someone will correct me, I am sure) that mosquitoes develop a resistance to DDT.
As mosquito-borne diseases continue to grow and expand, there is a knee-jerk reaction from governments, courtesy of the Friends of the Mosquitoes, to do little to nothing to combat the winged vector of diseases. Here in the Peoples' Republic of Tallahassee, the Leon County Commission bowed to the wild-eyed lunatic fringe, and imposed one of the most ludicrous acts in recent memory. If one single homeowner objected to the spraying for mosquitoes, then spraying would be abandoned for every parcel within a quarter-mile -- a quarter-mile! -- of that home. The effect was that 100 homeowners would effectively shut down mosquito spraying for almost all Leon County, Florida residents.
Former Leon Commissioner Ed DeDuy, a very good friend of mine, once said that few things arose as much passion as messing with mosquito spraying. And we was proven right again, as the silent majority of homeowners went apoplectic and raised such a ruckus that the commission flip-flopped and reversed the ban.
Those who oppose spraying for mosquito control strike me as in the same league as those who oppose vaccines because they (mistakenly) think they cause autism. Mosquito control is as much of a public health issue as vaccinating the population.
With West Nile Virus, Eastern Equine Encephalitis and Dengue fever, Florida is a contender for the Triple Crown of mosquito-borne diseases. Throw in some other diseases that hypothetically might be controlled by such spraying -- Lyme disease, for example -- and it is an imperative that we deal with these dangerous pests quickly and decisively. To paraphrase: Spray, baby, spray!
And bring back DDT. Let's abandon the junk science and save some lives.
Songbirds, not just fowl, represent avian flu threat to US
Over at Flutrackers, there is a thread regarding the prevalence of avian influenza in American birds.
Avian influenza virus (AIV) is an important public health issue because pandemic influenza viruses in people have contained genes from viruses that infect birds. The H5 and H7 AIV subtypes have periodically mutated from low pathogenicity to high pathogenicity form. Analysis of the geographic distribution of AIV can identify areas where reassortment events might occur and how high pathogenicity influenza might travel if it enters wild bird populations in the US. Modelling the number of AIV cases is important because the rate of co-infection with multiple AIV subtypes increases with the number of cases and co-infection is the source of reassortment events that give rise to new strains of influenza, which occurred before the 1968 pandemic. Aquatic birds in the orders Anseriformes and Charadriiformes have been recognized as reservoirs of AIV since the 1970s. However, little is known about influenza prevalence in terrestrial birds in the order Passeriformes. Since passerines share the same habitat as poultry, they may be more effective transmitters of the disease to humans than aquatic birds. We analyze 152 passerine species including the American Robin (Turdus migratorius) and Swainson's Thrush (Catharus ustulatus).
Methods
We formulate a regression model to predict AIV cases throughout the US at the county scale as a function of 12 environmental variables, sampling effort, and proximity to other counties with influenza outbreaks. Our analysis did not distinguish between types of influenza, including low or highly pathogenic forms.
Results
Analysis of 13,046 cloacal samples collected from 225 bird species in 41 US states between 2005 and 2008 indicates that the average prevalence of influenza in passerines is greater than the prevalence in eight other avian orders. Our regression model identifies the Great Plains and the Pacific Northwest as high-risk areas for AIV. Highly significant predictors of AIV include the amount of harvested cropland and the first day of the year when a county is snow free.
Conclusions
Although the prevalence of influenza in waterfowl has long been appreciated, we show that 22 species of song birds and perching birds (order Passeriformes) are influenza reservoirs in the contiguous US.
OK, insightful analysis time. We always associate bird flu with ducks, or chickens, or turkeys or geese, but rarely do we associate it with songbirds and other smaller birds. This study makes a clear association between those birds (called "passerines") and bird flu.
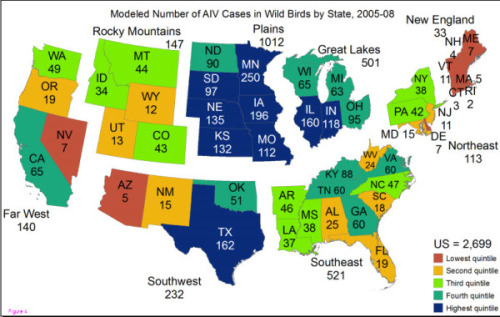
The distribution of those avian flu cases is seen in this map (thanks Laidback Al!):
Now let us look at a map of the principal migratory bird routes over North America:
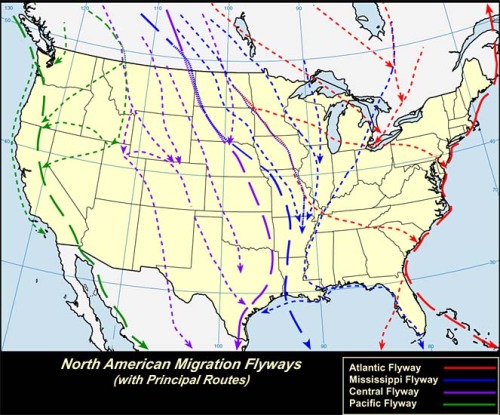
There is a veritable swarm of migratory bird routes over the Great Plains and Mississippi River delta, and a very strong west coast migratory route. So it is no coincidence, in my mind, that these migratory superhighways also contain the areas where avian flu has been most strongly detected since 2005.
Now you also notice those "down arrows" leading South of the Border. This map helps illustrate what happens south of us:

We've got birds encroaching from the south as well as from the north. This does not just figure into the avian flu equation: There is this little thing called a major dengue fever epidemic that is raging in many, if not most, South American nations. And as I mentioned recently, Key West, Florida has enough dengue in it to sicken a man this year.
This all leads into the current status of H5N1 sentinel activity. With massive budget cuts, waning interest, and competition for attention from swine flu and other diseases, do we have as good a handle on things as we did in 2006 and 2007? I would like to think so, but I doubt it.
Imagine the encounter: A researcher goes into his/her supervisor's office, requesting additional funds for H5N1 monitoring. What, the supervisor says? You want me to divert $$ from certain necessary projects over to bird flu monitoring? All while my departmental budget is being cut to ribbons?! No stinking way!
Or words to that effect. I wish it were not so, but I am pretty certain I am right.
In the midst of all this, the Mexican government recently issued an alert to be watchful for an H5/H1 hybrid virus. My first impulse was to say, What do they know? What have they heard? But is may have been nothing more than speculation. Nonetheless, vigilance is important, now more than ever. For H1N1v may not have been the pandemic everyone feared, but it was substantial in terms of its effect on the young; far worse than, say, 1977. Yet H1N1v, being 1/3 avian, can still hang out with avian flu viruses and reassort. It is precisely this scenario that should cause us to view this latest report with concern.
Trust Fineberg's committee to deliver accurate, relevant, honest WHO appraisal
Wow. It has been more than two months since my last blog entry. that must mean that H1N1v, or swine flu, is gone, right?
No. It means I am incredibly busy these days, and have not had much to say about pandemics nor about infectious disease. Well, that is not entirely true. For example, dengue fever has established a beachhold in Key West, Florida, where a Navy person recently was confirmed to have contracted dengue from within Key West's city walls.
Also, and as most of us surmised, swine flu is still worming its way through the developing world. India seems to be under the gun with outbreaks of H1N1v, and I am not sure what the genetic makeup of this new virus might be.
Additionally, recent reports regarding testing of the H1N1 vaccine on mice and subsequent attempts at infection with 1918 Spanish flu are encouraging. It appears that there is some conferred immunity from the 1918 pandemic virus with the H1N1 swine flu vaccine. This is important, because if you recall from reading this Blog, the 1977 recurrence of H1N1 was believed to be the result of a Soviet lab accident. So this pandemic may have been serendipitous in that it is helping immunize the planet against another Spanish Flu.
Anyway, the article that prompted me to write this blog actually deals with the WHO analysis of itself. The WHO has been the subject of much scrutiny as the result of what has been to date, a very mild pandemic. Some are inferring that Big Pharma actually orchestrated this pandemic in order to make a lot of money on vaccine and antivirals.
Believe me, Big Pharma has more and bigger things to make money on than vaccines. Anyone who really believes Big Pharma would drop everything it was doing to go and make vaccine just does not understand how drug companies make their money today. Druf companies see vaccine production as a necessary evil; a component of what they do, but not nearly as profitable as making and selling drugs dealing with everything from erectile dysfunction to hair loss.
In fact, accusing drug makers of profiting unnecessarily from vaccine production may actually cause drug makers to forego vaccine production in the future. Now some, including those misguided but WRONG individuals who think vaccines cause autism, might rejoice in that thought. But the simple truth is that drug companies see vaccine production as an important public health duty. And accusing them of orchestrating an overly aggressive response to a flu pandemic is placing blame in the wrong place.
Is there a right place to place blame? In my opinion, no. There is no blame. The WHO acted correctly. Now there are protocol adjustments to make, and my previous blogs have covered the principal problems, dealing with severity. The WHO needs to adopt the US "Saffir-Simpson" standard for pandemic severity. I am sure that concept will get an airing and eventual adoption.
But the absolute best news I gleaned from today's article about the WHO oversight committee deals with the committee itself. First, the AP story of today:
2 experts resign from WHO swine flu review panel
(AP) – 1 hour ago
GENEVA — The World Health Organization said Tuesday that two members of an expert panel reviewing the global body's response to the swine flu outbreak have resigned over concerns about perceived conflict of interest.
John MacKenzie and Tony Evans stepped down because their close association with the UN health organization during the outbreak could be seen as conflicting with the panel's ability to remain independent, WHO said.
"Both have been closely engaged in deliberations at WHO which our committee is charged to review," said panel chairman Harvey Fineberg. "They each concluded it would be better to avoid the position as reviewer of their own earlier actions."
Mackenzie, a professor of tropical infectious diseases at Curtin University in Australia, and Evans, medical chief of the Montreal-based International Civil Aviation Organization, were on the emergency committee that advised WHO's Director-General Margaret Chan before she declared swine flu a pandemic.
WHO convened the panel in April to conduct a "credible and independent review" of how it and national authorities handled the outbreak. Concerns were raised at the time that several panel members were trusted WHO advisers and government employees who could end up whitewashing any failures.
The review panel will present a final report next year.
Harvey Fineberg is Dr. Harvey Fineberg, head of the Institute of Medicine in Washington, DC. He also is the former head of the Harvard school of public health, and former Harvard provost. But to flubies, Harvey is best-known as the co-author of the seminal study of the 1976 swine flu debacle, along with the late historian Richard Neustadt. Harvey is also a pen pal of mine, and I engage him occasionally as a sounding board for ideas that, depending on his thoughts, eventually appear here as blogs.
Harvey may be the most-qualified person in the world to assess the WHO's handling of the 2009-10 swine flu pandemic. His 1976 study should be required reading for anyone who is interested in public policy when it comes to public health and infectious disease policy. I am equally certain his committee's analysis of the WHO's conduct during this latest pandemic will also be compelling reading.
Why Na Tao matters, despite apparent lack of human bird flu transmission
A reader of this Blogsite, Jonathan Singleton, asked me to comment on the recent proMED report regarding Na Tao, Vietnam. As you may know, Na Tao is at the heart of a possible cluster of human cases of bird flu. My previous two blogs have covered this developing situation.
The proMED report in question is below.
Influenza A (H5N1) is not transmitted from human to human
---------------------------------------------------------------------------
Yesterday afternoon [14 Apr 2010], at a meeting of the National Steering Committee for pandemic influenza control and prevention, Dr Tran Nhu Duong, Deputy Director of the National Institute of Hygiene and Epidemiology confirmed that influenza A (H5N1) has not been transmitted from human to human.
The investigation of the Institute on 2 cases of influenza A (H5N1) in Na Tao village, Nhu Co commune, Cho Moi District, Bac Kan province did not detect human to human virus transmission.
Reports of two investigation teams of the Institute in Bac Kan showed that the two patients were living about 100 meters apart, and they had never been in direct contact with each other.
All 33 people who had contact with the patients, including relatives, visitors, neighbors, nurses, and physicians, were tested and monitored for 16 days. There has been no case with symptoms of the disease. All the test results were negative.
Communicated by:
PRO/MBDS
As we now know, there are three suspected human cases, not two. But that is not material to our discussion. What is material is that two persons, living about a little more than a football field's distance apart, contracted H5N1 bird flu.
The report seems to conclude that distance alone, coupled with a lack of direct contact of one with another, eliminates the possibility of human-to-human (H2H) transmission. That sounds logical enough.
But the larger issue -- the proverbial elephant in the room -- is this: Has the virus itself changed enough in Na Tao, Vietnam, to allow for an easier method of transmission from avian to human respiratory cells? If so, that disclosure would prove to be almost as big (and ultimately more potentially troublesome) than another H2H cluster.
That is a question that the Vietnamese report does not answer.
Let's consider the facts. Three persons in one district contract bird flu. Apparently they all contracted it via contact with diseased poultry. That tells me that either the virus in that area of Vietnam is more potent, and/or the ability of the virus to favor human epithelial cells as much as it favors chicken epithelial cells.
We all know from reading the research papers that this proclivity toward one species or another is primarily driven by temperature. The fact that both diseased poultry and diseased villagers have been detected in a cluster bears investigating by the WHO. For a cluster is a cluster whenever you get multiple persons in a close area, H2H or no H2H. Three B2H bird flu cases in one hamlet should be significant enough to want to gather many samples and look at them very, very carefully.
